Woman 77 yo, by herself detected one lump at herleft breast.
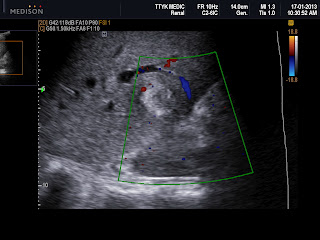
Ultrasound examination: this mass was at section of 10 hr of left breast, size arround 2 cm ( B mode US picture).
It was hypoechoic and irregular border, with very strong shadowing (image 2 and 3), and on CDI, hypervascular and very high PI.
On PDI again, this tumor was hypervascular; axillary scan no detected nodes.
Ultrasound first suggests breast cancer, next step ismammography or MRI.
THIS PATIENT REFUSED TO DO MAMMOGRAPHY AND MRI BECAUSE THE FIRST TECHNIQUE WAS PAINFUL AND THE SECOND ONE MADE CLAUSTROPHOBIA FOR HER LONG TIME AGO.
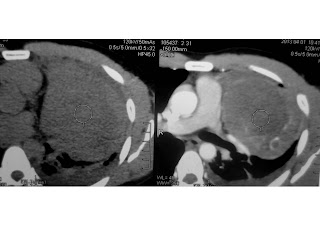
MSCT IS CHOSEN FOR STAGING THIS CASE. (SEE 3 CT SLICES )
MSCT non CE showed that tumor was small size of 1.8 cm, spiculate hypercalcification and detected no lymphatic nodes of axillary or retrosternum, it was staging I.
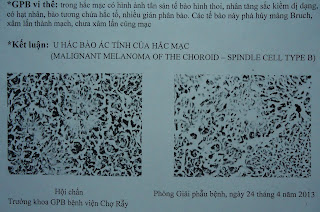
Biopsy was done and report was breast cancer type NOS.





.jpg)