Patient came to clinic with history of 3 years worsen polyarthralgia. He has been diagnosed and managed as degenerative arthritis in BacLieu Province Hospital for a year. The pain localized in left shoulder, right knee, hips and left ankle. Patient also experienced general fatigue and weight loss (5kg a year). MSK Ultrasound is indicated as first tool, goes along with blood tests.
Ultrasound of right knee: shows patient area of pain doesn’t come from joint but the bone. It exists erosion of periosteal of proximal tibia and hypervascularity in surrounding soft tissue. By switching to more penetrative linear probe, a hyperechoic bone mass is seen beneath periosteal erosion. Mass is homoechogeneity and has anechoic cysts inside.
Image 1: Erosion of periosteal of proximal tibia and hypervascularity in surrounding soft tissue
![]()
Image 2: A hyperechoic bone mass is seen beneath periosteal erosion. Mass is homoechogeneity with anechoic cysts inside. Second images shows normal articular cartilage and not fit for degenerative arthritis.
Ultrasound of left ankle:
Same condition as proximal tibia as in the distal end. Mass is better demonstrated with infiltrative border. During examination, patient feels imminent pain at place that probe compresses. Ankle joint is normal.
Image 3: Mass is better demonstrated with infiltrative border in distal end of tibia
Ultrasound of shoulder:
Shoulder rotator cuff are normal. Area of pain is at left A-C joint. In comparison to normal right side, same apperance of bone mass revealed at clavicular end.
Image 4: Shoulder rotator cuff are normal. Area of pain is left A-C joint. In comparison to normal right side, same bone mass at clavicular end revealed.
Conclusion : Multiple distal bone masses suggest few differential diagnosis: Metastasis, Multiple myeloma metastasis.
Those could be pseudo-mass coming from bone erosion in osteclastic hyperactivity in hyperparathyroidism. Althought the lesions are common in middle diaphysis but not in the distal/proximal end. Radiologist did a quick check on the neck to rule out tumor of parathyroid gland.
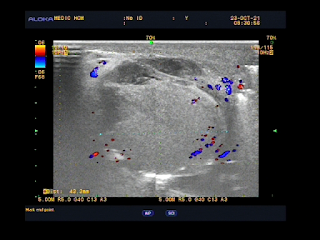
Ultrasound of the neck: detected at right lower lobe of thyroid a parathyroid tumor, 3.7x1.4mm, enlarged with capsule and hypervascular on colour Doppler mode.
Image 5: Right parathyroid tumor, 3.7x1.4mm, enlarged with capsule and hypervascular signals on colour Doppler mode.
Image 6: Pelvis X-Ray: shows multiple scattered oval-shaped bone radiolucent, losing bone general density.
Image 7 : Right ankle XRay: radiolucent oval-shaped lesion at distal tibia end in comparison to ultrasound.
Image 8: Right ankle XRay: radiolucent erosion lesion at distal clavicular end as compared to ultrasound.
Patient is preferred to endocrinologist and full body scan to perform looking for bone fracture as common complication because patient suffering illness for a long time.
Patient blood tests confirmed diagnosis: hypercalcemia and normal RF quantitative. Serum PTH value elevated >1200
Patient underwent surgery to remove the tumor. Pathological result : Parathyroid adenoma.
After the surgery, PTH value drops to normal value, serum calcium also drops below normal line and had been got oral calcium supply as he discharged from hospital.
Follow up on 3 months later, patient recovered and experienced no pain. He has already can go back to work.
Discussion and conclusion:
Primary hyperpaprathyroidism is caused by parathyroid tumor excretes PTH. That activates re-absortion calcium in kidneys, increase absorption in colons and bone loss. Osteoclastic hyperactivity produces subperiosteal erosions, endosteal cavitation and replacement of marrow spaces by vascular granulations and fibrous tissue. Brown tumor is known as Osteoitis fibrosa cystica. Pseudo-tumour, fluid-filled cysts contents hemorrhage and giant cell wrap within fibrous stroma. Giving rise to brownish, tumour-like masses. The lesion can be single or multiple. Well-defined and commonly affecting the facial bone, pelvis, ribs and femoral bone. The classical which should always be sought is sub-periosteal cortical resorption of middle phalanges.
But bone lesions in tibia end and clavicle ends of this case seem not to be so classical findings (in diaphysis instead).